Integrated planning: why medical schools need a joined-up approach
The pandemic has forced those involved in learning and research to reassess their methods and rapidly deploy new innovations in training and discovery. Nowhere has this been as profound as in Schools of Medicine, says AECOM’s Mark Whiteley.
Emerging from the pandemic, the medical schools that leverage lessons learned from operating at an unimaginable pace and with so much resilience and creativity will be the ones to lead the field. The question they should be asking is, “how do we build these new behaviors and processes into our organization so that we continuously raise standards in education and research in the years ahead?” The answer is integrated strategy.
In the past, planning was siloed with aspects of research, learning, business, operations and facilities addressed separately. In contrast, planning of the future will be integrated – embracing joined up thinking, increased collaboration and data-driven decision making.
In this article, we identify six important aspects that are driving transformative initiatives in academic medicine. Even in the midst of the pandemic there are schools across the United States that are already reimagining their future by addressing these core themes. Strategy+, AECOM’s design-led management consulting studio has been working with these institutions to implement these approaches, and we include some of these case studies below.
 1/SYNCHRONIZED
1/SYNCHRONIZED
By aligning streamlined processes and policies, innovative activities, inclusive governance structures, new partnerships and service models with optimized resource allocation we can more effectively target the delivery of innovative real estate. To do this however, organizations need to move away from traditional siloed approaches where the focus tends to be on individual projects or processes. In contrast, taking a synchronized approach means aligning shared learning, research and administrative resources for greater efficiency. Using an inclusive governance structure, planning and communication can be synchronized. Organizational improvement can dramatically reduce change the need for space.
CASE STUDY: Lehigh University’s New College of Health engaged Strategy+ to design and implement a shared services model that leverages a ”concierge” capability. Cross-trained professionals are allocated a faculty group and provide personal-focused assistance in aspects of HR, student support, research pre- and post-award support, tech transfer and marketing.
 2/DYNAMIC
2/DYNAMIC
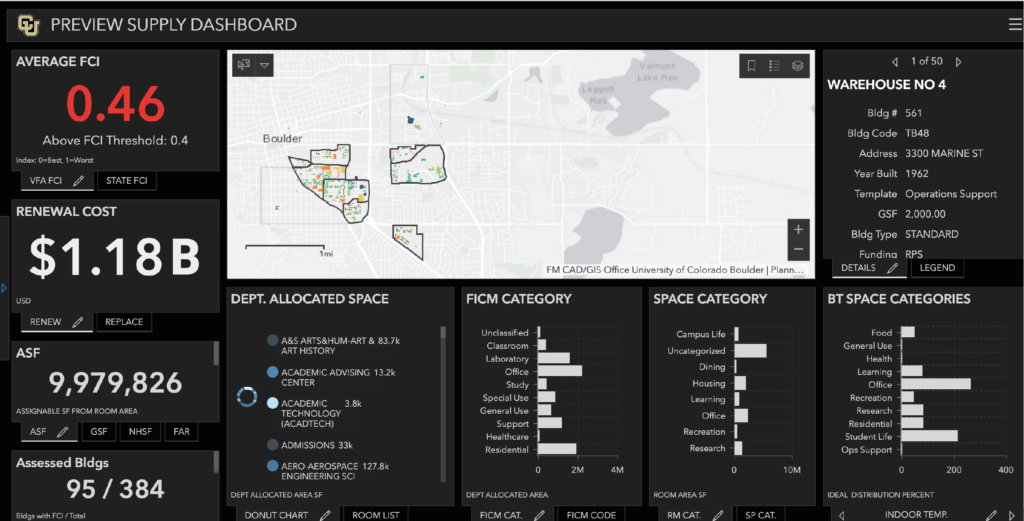
Taking a dynamic approach means leveraging mission-driven live analytic dashboards to make informed decisions on enrollment, research performance and future capital investments, rather than taking a static, non-data-driven approach that represents just one point in time. Interactive planning tools driven by live databases allows us to undertake real time modelling of changes in enrollment, pedagogy, new programs and research expenditures, and see the effect on financial, physical, human and technological resources.
CASE STUDY: University of Colorado, Boulder has engaged Strategy+ to create an interactive GIS academic planning tool. It facilitates the analysis of enrollment, revenue and costs, human resources, facility suitability, space utilization, new pedagogies, operating costs, and income generation to assess real estate solutions capacity to address evolving learning and research opportunities.
 3/DIGITAL
3/DIGITAL
The global pandemic has forced new learning, working, research and clinical practices to become mainstream and in response institutions are learning to look beyond their physical infrastructure. Moving forward, institutions must learn to leverage agile mobile working practices, and continuously adopt new technology and update curriculums to improve accessibility, efficiency and quality of multi-modal learning. For example, first- and second-year students have focused on virtual anatomy and interacting with standardized patients on-line. Third and fourth years learn on-line in redesigned clerkships involving faculty-guided, didactics and patient videoconferences. Digital infrastructure has increased faculty and staff mobility who can now work anywhere.
CASE STUDY: The University of California’s Riverside School of Medicine engaged Strategy+ to integrate collaborative digital experiences into its future education facility. For clinical skills we realigned contact hours for small groups in virtual anatomy, virtual standardized patients and i-human encounters. We also realigned its workplace strategy to integrate mobile teaching and administration.
 4/MISSION-DRIVEN
4/MISSION-DRIVEN
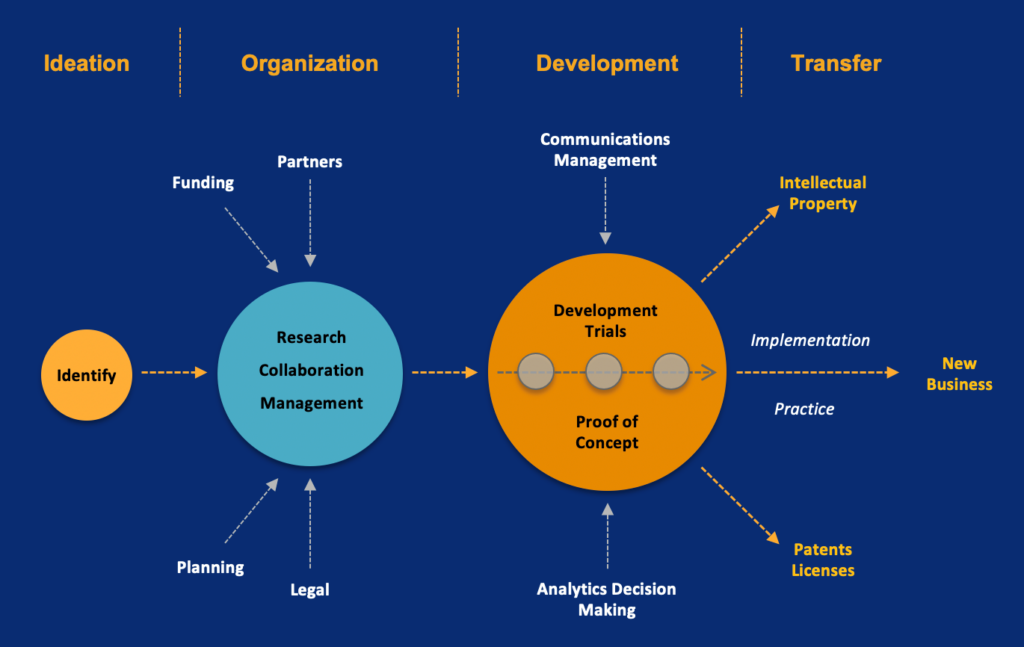
Colleges of medicine are increasingly using mission-focused strategic initiatives and metrics-driven goals to define their brand and focus their academic vision. Mission-driven planning develops these academic, financial, operational and experiential differentiators into a timeline of metrics-based targets that drive the types and extent of optimal research and learning facilities. This marks a shift away from traditional planning-driven approaches that focus on development sites and their phased delivery.
CASE STUDY: NYIT College of Osteopathic Medicine asked Strategy+ to develop research and technology transfer focus areas as part of its strategic plan. Leveraging its strengths in anatomy, esports and comprehensive whole person practice they will concentrate on recruiting osteopathic research specialists and grow targeted research income.
 5/TRANSFORMATIVE
5/TRANSFORMATIVE
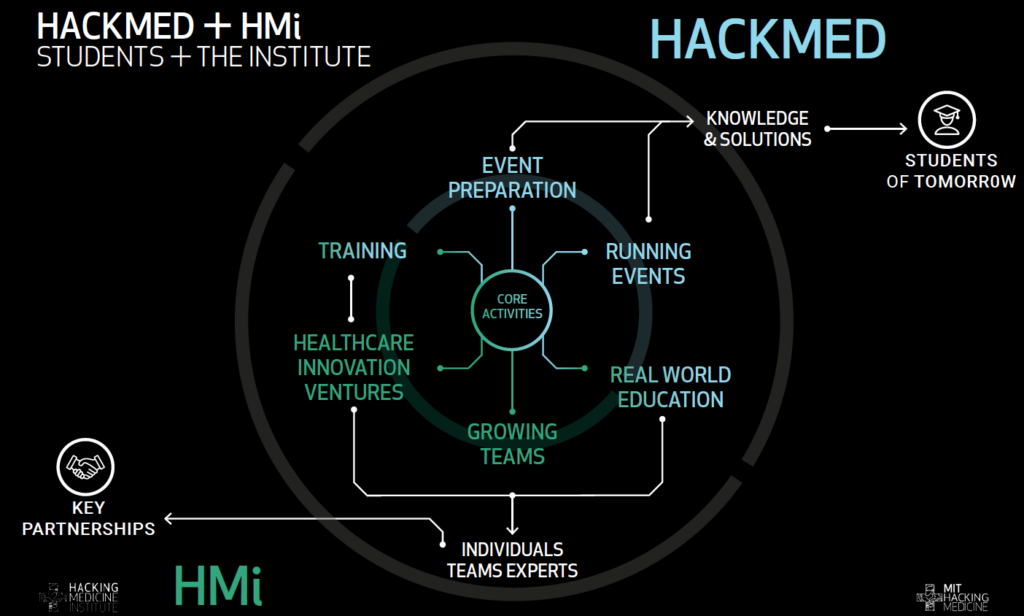
The pandemic has emphasized the need to reassess traditional programs, curriculum and student support delivery modalities. New approaches to the social determinants of health, public health, population health and telemedicine are driving new forms of inter-professional teaming. This is in contrast to traditional approaches where consultation and collaboration occurs solely within the organization.
CASE STUDY: MIT Hacking Medicine Institute (HMi) As a dramatic departure from how MIT currently leverages its work into outcomes and impact, HMi’s vision, virtual operational model, governance structure and funding strategy is intended to disrupt the health industry by crowdsourcing targeted health related challenges and accelerating solutions to market.
 6/OUTCOME-BASED
6/OUTCOME-BASED
It’s not enough to just take an aspirational approach. Goals must have targets. Equate your initiatives and facility decisions with metrics for equity, diversity, inclusion, economic mobility, workforce needs and community impact. Medical schools are employers – they support populations and undertake research activity that has major economic and social impact. Outcomes-based planning focuses not only the implications that investment decisions have on facilities and infrastructure, but also on regional economics, workforce needs and livability.
CASE STUDY: University of Texas Rio Grande Valley Medical School (UTRGV) required a roadmap for regional education, health and economic development. Their plan directly relates the provision of cost-effective medical education, the creation of industry-focused R&D clusters and growth of health science programs to provide economic impact, improved health outcomes and enhanced cultural enrichment.
About Strategy+